The 2025 ISR Benchmarking Report, based on independent sponsor evaluations, named Rave EDC the #1 preferred EDC.
The Medidata Experiences
Our Suite of Products & Solutions
Medidata is the leading provider of SaaS and data analytics solutions that support clinical research. Discover how our products and services help advance all stages of your clinical trial.
Medidata Platform
The industry’s only unified platform dedicated to clinical research—proven to transform trials.
Data Management
Next-generation solutions that eliminate complex, manual processes for higher quality data and faster insights.
Trial Management
Accelerate study timelines from planning to close with connected workflows and centralized insights.
Patient Engagement
Powerful, patient-facing technologies that make clinical trials simple and engaging for patients.
Professional Services
Comprehensive support designed to drive exceptional customer engagement for a best-in-class experience.
Evidence Generation
Unparalleled trial data combined with advanced analytics and deep human expertise—all on a single platform.
Healthcare Solutions
Exchange EHR and other healthcare data to power a new level of collaboration and patient care.
Decentralized Trials
Decentralizing solutions on a unified platform for patients, sites, and sponsors.
A Few of Our Partners & Customers
“Our partnership with Medidata has enabled us to offer top-notch service to sponsors. In the last decade, we’ve embraced the latest Rave EDC technology, including eCOA/ePRO via the Patient Cloud and Rave Coder. We’ve successfully configured intricate study designs, from early-phase oncology with numerous protocol changes to rare disease studies with diverse data collection methods.”
– Melissa Hancock, Director, eClinical Technologies

“The team of Professional Services that I work with is very intelligent and collaborative…. We enjoy working with Medidata, it’s a great team. They’re always willing to come to the table and discuss our needs.”
– Heidi McIntyre, Director of Centralized Data Monitoring, Moderna

“…the Medidata products are very innovative and support our very complex oncology studies…”
– Vijay Chundru,Senior Director, EDC Programming Team, Global Clinical Data Operations, Jazz Pharmaceuticals

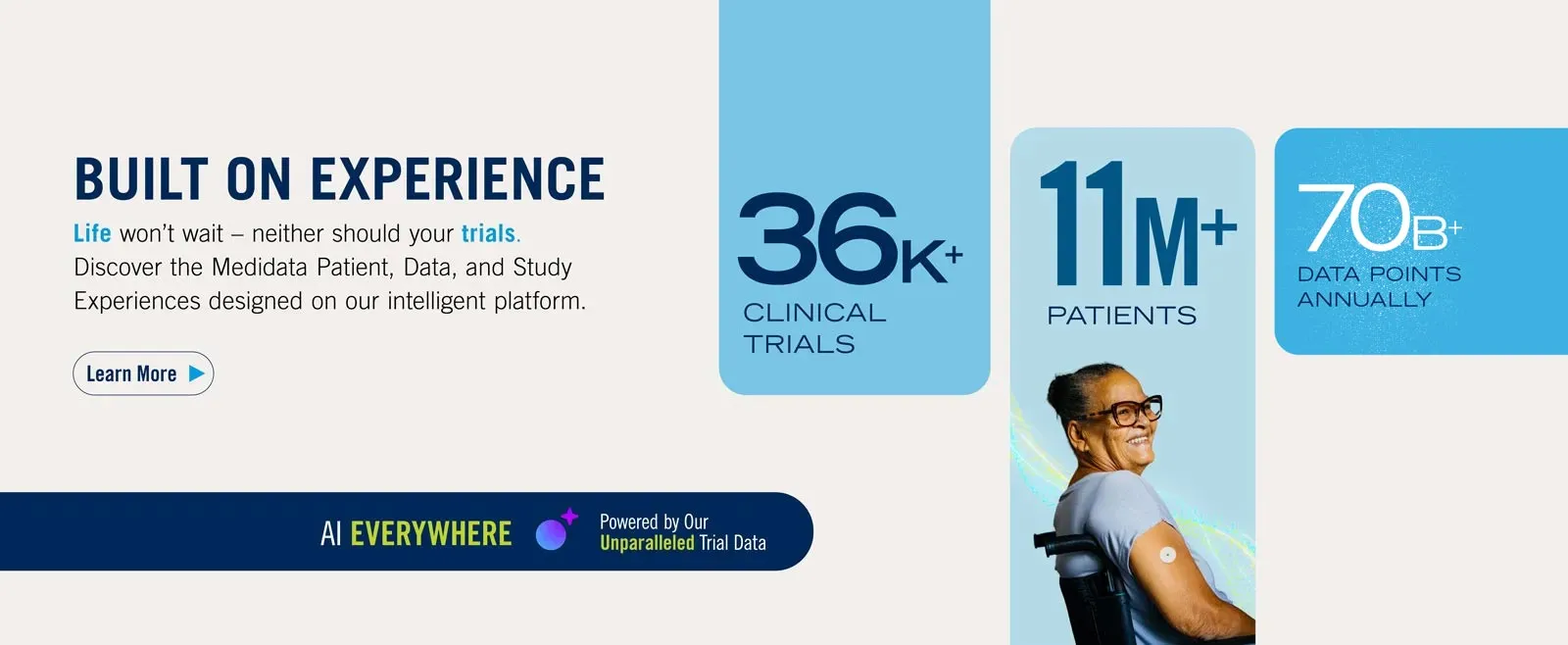
Built on Experience
Medidata harnesses AI and our unparalleled trial dataset from over 25+ years of global collaboration to power smarter treatments and healthier people.
Clinical Trials
Thousands of studies in 140+ countries have been conducted on the Medidata platform.
Patients
Over 11 million patient participants across Medidata trials have impacted clinical research and touched countless lives.
Customers
Medidata studies, patients, and data are involved in 26% of company-initiated trial starts globally.
FDA-approved novel drugs
Medidata supported 72% of 2024 FDA novel drug approvals and 62% since 2015*.
*Excludes vaccines and biologics
Industry Insights
Discover the latest life sciences breakthroughs with insights and expertise from our thought leaders.
Contact Us
Ready to transform your clinical trials? Get in touch with us today to get started.